We bring practical, collaborative CPD to rural health professionals where it’s needed most — across rural, remote and Indigenous communities in British Columbia.
As UBC Rural Continuing Professional Development (CPD) wraps up the 2024-25 learning season, we reflect on the impact of our work with the Rural Coordination Centre of BC (RCCbc).
This past year, we delivered:
- 45 plans completed through Personal Learning Plans (PLP).
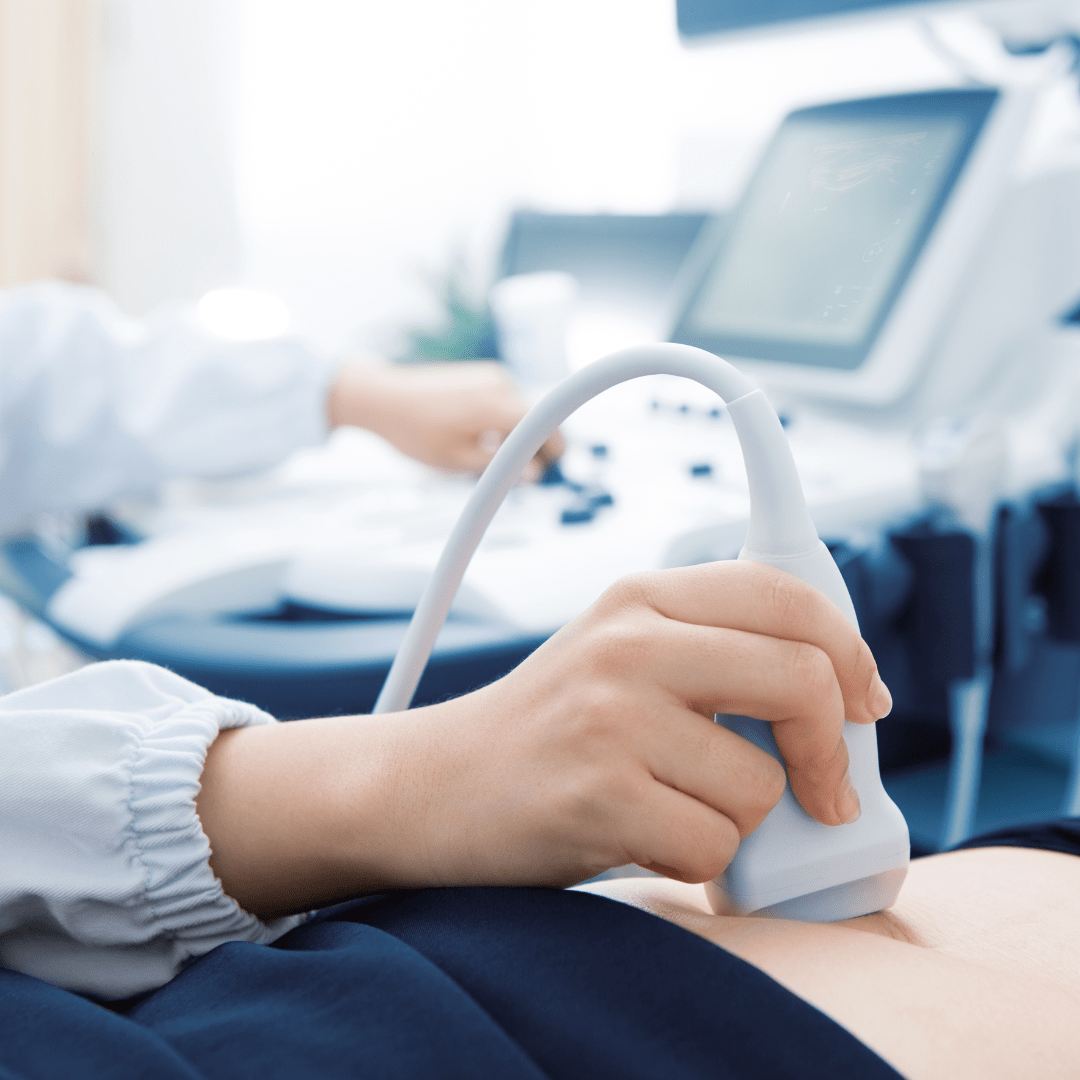
- 17 Hands-on Ultrasound Education (HOUSE) course days, reaching 115 learners in rural communities.
- 26 Real-Time Virtual Support (RTVS) Simulation sessions.
- Eight synchronous Rural Rounds virtual webinars, reaching 409 learners.
- Five synchronous Virtual Health Grand Rounds (VHGR) webinars, reaching 273 learners.
- 1351 mentoring hours in the Coaching and Mentoring Program (CAMP), with 432 active participants.
- Level 1 and Level 2 Nawh whu’nus’en — We see in two worlds workshops in the Indigenous Patient Led (IPL) CPD program, with 399 total attendees.
Multi-modal learning opportunities
The Hands-on Ultrasound Education (HOUSE) program launched its first Rural Point-of-Care Ultrasound (POCUS) Congress in 2024, tackling popular topics on trauma, procedures and critical care.
A new Intro to Cardiac session was also introduced in the Rural POCUS Rounds monthly virtual series, helping physicians improve POCUS skills and patient care.
“Fantastic webinar, very useful tips, great presenter and moderator!” says one participant.
The Rural Rounds Education Hub partnered with new subject matter experts to deliver a unique session, Doctor and Friend: Navigating Care Boundaries in the Rural Setting, addressing challenges in rural health communities.
Virtual Health Grand Rounds (VHGR) continued its quarterly webinar series to bridge technology and health care. A new session Reimagining Virtual Care Through Patient Partnership explored how virtual care can be shaped through patient involvement.
In Fort. St. John, British Columbia, the Real-Time Virtual Support (RTVS) Simulation program delivered five simulations focused on maternity, pediatrics and emergency care.
Cultural humility and meeting the needs of Indigenous patients and families
Over 500 learners have now completed the Level 1 Nawh whu’nus’en: We see in two worlds course in our Indigenous Patient Led (IPL) CPD program. This milestone inspires the Rural CPD team to continue education development on culturally safe care for Indigenous peoples in rural areas.
Fostering meaningful professional relationships
The confidential Personal Learning Plans (PLP) program connects new-to-rural practice physicians and International Medical Graduates (IMGs) with experienced physician advisors. Read the recent story on PLP.
Through the Coaching and Mentoring Program (CAMP), participants received over 1350 hours of tailored coaching and mentoring this year.
"Having feedback from someone with a lot of experience was crucial. It gave me the ability to improve and maintain a high level of care,” says a 2024 CAMP participant.
Looking ahead
UBC Rural CPD remains dedicated to supporting lifelong learning for rural health professionals. Guided by a passionate team of physicians and CPD professionals, we deliver education based on lived experience of those practicing in rural, remote and Indigenous communities in British Columbia.
“As we reflect on this past year, we want to extend our gratitude to everyone who makes our work at Rural CPD possible,” says Dr. Dana Hubler, Medical Director, Rural CPD.
As we plan for the year ahead, we are excited to continue this important work.
Help shape future learning by completing the short, anonymous Rural CPD Needs Assessment Survey.
Read the full 2024-2025 Rural CPD Annual Report.
Partners
UBC Rural CPD was established in 2008 and operates in partnership with the Rural Coordination Centre of BC (RCCbc). Funding for the program is provided by the Joint Standing Committee on Rural Issues, a joint committee of the Doctors of BC and BC Ministry of Health.